Schizophrenia
From Psy3242
Ceisenbrandt (Talk | contribs) |
Sriegsecker (Talk | contribs) |
||
| Line 24: | Line 24: | ||
The exclusion criterion describes conditions that prevent a diagnosis even if the core symptoms and course criteria are present. For example, a patient with marked disruptions of mood would qualify them for a mood disorder rather than a diagnosis in schizophrenia. A diagnosis can also not be made if an external physical cause is what triggers the mental disturbance. For example, excessive drug use and neurological conditions such as epilepsy may elicit schizophrenic-like symptoms. | The exclusion criterion describes conditions that prevent a diagnosis even if the core symptoms and course criteria are present. For example, a patient with marked disruptions of mood would qualify them for a mood disorder rather than a diagnosis in schizophrenia. A diagnosis can also not be made if an external physical cause is what triggers the mental disturbance. For example, excessive drug use and neurological conditions such as epilepsy may elicit schizophrenic-like symptoms. | ||
Two of the most common systems used for diagnosis are the ICD and DSM-IV. The International classification of diseases or ICD was created and is maintained by the World Health Organization and is currently on its 10th edition. | Two of the most common systems used for diagnosis are the ICD and DSM-IV. The International classification of diseases or ICD was created and is maintained by the World Health Organization and is currently on its 10th edition. | ||
| - | Another system commonly used for diagnosis measures is the American Psychiatric Association’s Diagnostic and Statistical Manual or DSM-IV. If the | + | Another system commonly used for diagnosis measures is the American Psychiatric Association’s Diagnostic and Statistical Manual or DSM-IV. If the conditions stated in this manual are not met a patient should not receive a diagnosis. |
==Causes== | ==Causes== | ||
Revision as of 04:03, 28 April 2008
Contents |
Schizophrenia (skiht-zo-FREH-nee-uh)
Definition
Schizophrenia is a thought disorder that affects about 1-2% of the human population each year. While it remains uncertain what the cause of the disease is, several studies suggest heredity to be a main component. There are two types of schizophrenia. Type I or acute schizophrenia involves hallucinogenic and delusional experiences along with a distortion of thought processes. Type II, or chronic schizophrenia is the most severe classification of the disorder, involving a reduction or elimination of normal mental and/or behavioral processes. A cure for the disease is yet to be found, however some antipsychotic drugs can be useful in controlling type I symptoms.
History
The first clinical descriptions of schizophrenia date back to as early as 1809. John Haslam and Philippe Pinel at this time released books on mental illnesses that contained the first complete reports of what is now know as chronic or type II schizophrenia. Haslam’s Observations on Madness and Melancholy documented the first historical description of schizophrenia in the English language. Alois Alzheimer conducted the earliest known neuropathological studies of Dementia Praecox. The German psychologist published his findings in 1887. Alzheimer along with Nissi Franz collaborated with Emil Kraepelin in what is now known as the first multi-disciplinary research program. Kraepelin believed there was a specific biological cause for major psychiatric disorder; therefore their research was focused on this belief. Kraepelin was the first to divide the originally unitary concept of psychosis into two forms, manic depression (now know as bi-polar disorder), and dementia praecox (now known as schizophrenia). Kraepelin was the introduced his original concepts in the 4th edition of his book Lehrbuch der Psychiatrie in 1893. It was in this book that he defined dementia praecox as “a sub-acute, development of a peculiar, simple condition of mental weakness occurring at a youthful age.” He also discussed the importance of his method of recognizing patterns rather than grouping symptoms as a means for determining a diagnosis. In 1908 Eugen Bleuler redefined dementia praecox and coined the term schizophrenia. Bleuler realized the condition was neither a ‘dementia’ nor did it only occur in young individuals (praecox meaning ‘early’), as Kraepelin had originally suggested. The term schizophrenia is a combination of the Greek words schizo meaning ‘splitting’ and phrenia meaning ‘mind’. The literal translation of the term is ‘suffering from a split mind.’ Bleuler provided a new perceptive of the disease in his 1911 book Dementia Praecox oder die Gruppe der Schizophrenien. Along with redefining schizophrenia, as it is known today, Bleuler also know for assisting in the discovery of Alzheimer’s disease. It should also be noted that Bleuler himself suffered from the psychological syndrome, Synesteasia. From 1920s to late 1960s psychoanalysis dominated American Psychiatry causing a lack of research and development in the biological realm of Psychology. However, advances in technology in the 1970s allowed for new research in biochemistry, brain function and structure, genetics and the development of brain imaging techniques lead to a revival of studies on schizophrenia and other psychological disorders. Schizophrenia began to be referred to as a ‘brain disease’ and after years of neglect, the search for the causes of schizophrenia was once again a highly prioritized topic for research. It is now a century after Bleuler introduced schizophrenia and there is still not a universally accepted definition for schizophrenia or a known cause for the condition. However, a standardized criterion for diagnosing the condition has been developed.
Symptoms
Schizophrenia can be described in terms of primary and secondary symptoms. Primary symptoms were those involved in indicating thought disorder and/or emotional blunting. Emotional blunting is Bleuler’s term describing the inability to experience normal emotions. Primary symptoms, more recently referred to as ‘negative’ symptoms, are those that cause an individual has an impaired relationship with the external world. Negative symptoms are evident in Type II schizophrenia, the most severe form. Secondary, or ‘positive symptoms’, involve an individual experiencing hallucinations and/or delusional beliefs. A patient with primarily positive symptoms is described as having a Type I, or less severe case of the syndrome. Positive symptoms are the most identifiable symptoms of schizophrenia in their expression. They are referred to as being ‘positive’ because the syndrome produces or ‘adds’ abnormal events such as experiencing a sensation in the absence of something to be sensed in the environment. Delusions or beliefs based on false information are also common symptoms along with uncontrollable thought patterns. Positive symptoms are considered a class of thought disorder and speech abnormalities that take form in an inability to make associations in thought processes. A schizophrenic experiencing speech abnormalities may often make illogical conversation in which the connections between ideas are disjointed or non-existent, at least to the listener. A speech patient’s conversation may come out as nothing but an incomprehensible mixture of words. A patient may also jump to conclusions or ahead of their own thoughts as a result of following their own strange thought processes. Patients experiencing thought disorders often provide complex responses in the form of rambling to simple ‘yes or no’ answer questions. Negative symptoms are those involving the reduction or in some cases, elimination of normal mental or behavioral processes. Negative symptoms are evident in Type II schizophrenics. Dr. Nancy Andreason created a classification system of the predominant symptoms of Type II schizophrenia. These symptoms include: poverty of speech or Alogia, restricted affect and diminished emotional range, diminished interest in environment and reduction in curiosity, diminished sense of self purpose, and diminished interest in social interaction with others.
Diagnosis
In order for a patient to be diagnosed with Schizophrenia 5 major criteria must be present from 2 groupings: core symptoms and course criteria. A 3rd grouping also affects the diagnosis is the exclusion criteria, if any factor from this grouping is indicated by the patient schizophrenia cannot be diagnosed. The core symptoms criterion requires the presence of extreme disruptions of thought, perceptions, emotions, and motor behavior. These symptoms must occur for a significant portion of a one-month time period. These disruptions may take form of delusions and/or hallucinations and must occur with disturbances of speech or motor activity, and/or a disturbance of emotional responses. The course criterion requires symptoms and behavioral aspects to follow a specific pattern during a certain time sequence. This time sequence differs depending on the system used for diagnosis. The course criterion requires the core symptoms to be associated with impaired functioning in the patient’s daily life. The exclusion criterion describes conditions that prevent a diagnosis even if the core symptoms and course criteria are present. For example, a patient with marked disruptions of mood would qualify them for a mood disorder rather than a diagnosis in schizophrenia. A diagnosis can also not be made if an external physical cause is what triggers the mental disturbance. For example, excessive drug use and neurological conditions such as epilepsy may elicit schizophrenic-like symptoms. Two of the most common systems used for diagnosis are the ICD and DSM-IV. The International classification of diseases or ICD was created and is maintained by the World Health Organization and is currently on its 10th edition. Another system commonly used for diagnosis measures is the American Psychiatric Association’s Diagnostic and Statistical Manual or DSM-IV. If the conditions stated in this manual are not met a patient should not receive a diagnosis.
Causes
While the cause of schizophrenia remains uncertain, there are several widely supported theories. Two dominating perspectives as to what might cause schizophrenia are a biological hypothesis and a collaboration of several neuropathological hypotheses.
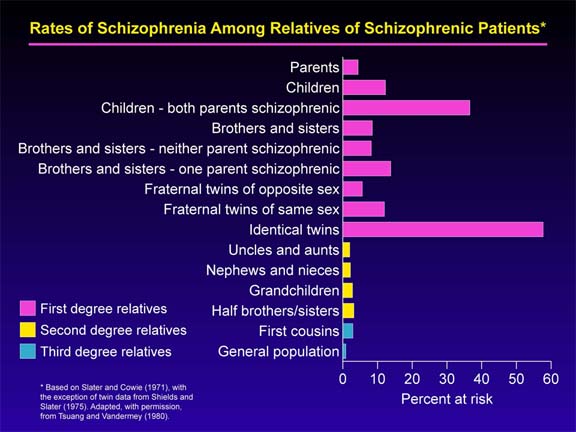
Biological Hypothesis: One of the most prevalent theories for the cause of schizophrenia is heritability. Numerous studies provide evidence that genetics may be behind the condition. The evidence behind this theory comes primarily on epidemiology, family studies, adoptive studies, and twin studies. Studies have shown 10% of children who have a single schizophrenic parent develop the condition, while 50% of children from parents both suffering from the disease manifest schizophrenia in its more severe form. Twin studies provide the most insight into how big a role genetics plays in developing schizophrenia. It is difficult to prove in that similar familial environments could also have an affect on the development of the condition. However, twin studies have provided important evidence to support the heritability theory. 33-78% of monozygotic twins both develop schizophrenia while only 10% of dizygotic twins develop the disease. Dizygotic twins have the same likelihood to develop schizophrenia as any offspring of a schizophrenic case. However, studies have shown monozygotic or identical twins are much more likely to develop the condition. In edition, studies have provided evidence that monozygotic twins raised in separate familial environments are more similar in personality than monozygotic twins raised in the same familial environment. A study has not yet been conducted of a pair of monozygotic twins suffering from schizophrenia, but it could provide the information necessary to prove or disprove this theory. While many researchers are convinced heritability plays a factor in the development of schizophrenia, the large body of evidence has supported no singe locus model of transmission.
Neuropatholigical Hypotheses: The most prominent experts in the field of schizophrenia cannot come to agree upon the interpretations of almost every neuropathological finding. Therefore, a cause for the syndrome has not yet been distinguished. However, studies have provided some insight into what the most probable causes could be. There are two ways of gaining neurological evidence. The first is referred to as macroscopic in which the larger structures of the brain are observed and measured. While histological, the second means, involves microscopically examining the structure and neurochemistry of the types of cells in the brain. For example, a histological study of the brain may involve the study of neurons in the brain. In 1999, Paul J. Harrison published an article in the scientific journal, Brain that provided a comparison of various claims to the cause of schizophrenia. In this article, Harrison provided a list of macroscopic and histological findings. Harrison’s list is presented in decreasing level of certainly. For example, the first finding listed has the most neuropathological evidence behind it. Strongest macroscopic findings:
1. Enlarged lateral and third ventricles of the brain, the ventricles are the spaces between the lobes where cerebrospinal fluid flows.
2. Decreased cortical volume or having a smaller, lighter brain. Enlarged ventricles and decreased cortical volume has been noted in people’s first schizophrenic experience, suggesting that the brain abnormalities are not caused by any sort of treatment for the disease and are not caused by the progression of the disease because they are present at the onset of schizophrenia. This supports the notion that people who develop schizophrenia have structurally abnormal brains before experiencing schizophrenic symptoms. 3. The temporal lobe loses more volume than other areas of the brain 4. Decreased thalamic volume, major relay center for sending messages in the brain has been found to be smaller and lighter in those with schizophrenia. 5. The shrinkage of the brain seems to occur in the ‘gray’ matter of the brain that is mostly made of neurons Strongest Histological findings: 1.Absence of gliosis as an intristic feature 2. Smaller cortical and hippocampal neurons 3. Fewer neurons in dorsal thalamus 4. Reduced synaptic and dendrite markers in hippocampus 5. Misdistribution of white matter neurons 6. Entohirnal cortex displexia 7. Cortical or hippocampal neuron loss 8. Disarray of hippocampal neurons