Female reproductive
From Iusmhistology
(Difference between revisions)
(→The uterine cycle) |
|||
| Line 369: | Line 369: | ||
*Proliferative stage: | *Proliferative stage: | ||
**Recall that during the proliferative stage, a follicle in the ovary is maturing to secondary and Graafian stage and producing more and more estrogen and progesterone. | **Recall that during the proliferative stage, a follicle in the ovary is maturing to secondary and Graafian stage and producing more and more estrogen and progesterone. | ||
| - | **The | + | **The proliferative stage is '''driven by estrogen''' produced by the developing follicle. |
**The proliferative stage is characterized by '''resurfacing of the endometrium through epithelial and stromal proliferation'''. | **The proliferative stage is characterized by '''resurfacing of the endometrium through epithelial and stromal proliferation'''. | ||
**This resurfacing requires the lengthening of the uterine glands and is accompanied by '''coiling of the glands'''. | **This resurfacing requires the lengthening of the uterine glands and is accompanied by '''coiling of the glands'''. | ||
| Line 380: | Line 380: | ||
**Recall that during the secretory stage the ovary has generated a corpus luteum and is producing estrogen and progesterone. | **Recall that during the secretory stage the ovary has generated a corpus luteum and is producing estrogen and progesterone. | ||
**Recall that the secretory stage takes place after ovulation and lasts until the corpus luteum degenerates or pregnancy is terminated. | **Recall that the secretory stage takes place after ovulation and lasts until the corpus luteum degenerates or pregnancy is terminated. | ||
| - | **The secretory stage is '''driven by progesterone from the corpus luteum | + | **The secretory stage is '''driven by progesterone''' from the corpus luteum. |
**The secretory stage is characterized by '''release of glycoprotein-rich products''', '''swelling and torture''' of the glands and spiral arteries, and '''accumulation of fluid in the stroma''' of the endometrium. | **The secretory stage is characterized by '''release of glycoprotein-rich products''', '''swelling and torture''' of the glands and spiral arteries, and '''accumulation of fluid in the stroma''' of the endometrium. | ||
*Ischemia: | *Ischemia: | ||
| - | + | **Recall that during the ischemic stage the ovary is seeing low hormone levels and the degeneration of the corpus luteum. | |
| + | **Note that the ischemic stage does not occur when pregnancy is initiated by implantation and the placenta maintains estrogen and progesterone levels. | ||
| + | **The ischemic stage is characterized by '''constriction of the coiled arteries''', '''stromal fluid loss''', and '''lymphocyte / macrophage cell invasion'''. | ||
| + | ***Recall that '''progesterone inhibits prostaglandins''' and that '''prostglandins are potent vasoconstrictors'''. | ||
| + | ***When the corpus luteum degenerates and progesterone levels drop, local prostaglandins are released into the endometrium. | ||
| + | **The coiled arteries dilate and constrict intermittently which causes ischemia, cell lysis, a weakened stroma, bursting vessles, and debridement of the functionalis. | ||
====Uterine cervix==== | ====Uterine cervix==== | ||
| + | *As mentioned before, '''the cervix is histologically distinct''' from the rest of the uterus. | ||
| + | |||
| + | *The cervical mucosa: | ||
| + | **The cervical mucosa of the uterus is not shed at menstruation like it is along the rest of the uterus. | ||
| + | |||
| + | *The cervical myometrium: | ||
| + | **'''The cervical myometrium has '''less smooth muscle''' and '''abundant collagenous connective tissue with elastic fibers'''. | ||
| + | |||
| + | *The cervical endometrium: | ||
| + | **The cervical endometrium has '''denser stroma''', '''simple columnar epithelium''', '''branched, dilated, cyst-forming glands''', and longitudinal mucosal folds called '''plicae''' (plicae palmatae). | ||
| + | ***Cervical glands can form cysts called '''Nabothian cysts'''. | ||
| + | |||
| + | *The cervical mucus: | ||
| + | **The cervical mucus changes throughout the uterine cycle. | ||
| + | **Mid way through the cycle (think ovulation and sperm-friend environment) the mucus is '''watery''', contain '''lysozyme''' (bacterioalcidal), and promotes sperm motility. | ||
| + | ***This sperm-friendly mucus is '''estrogen-stimulated'''. | ||
| + | **Late in the uterine cycle (think corpus luteum and potential implantation) the mucus is viscous and '''progesterone-stimulated'''. | ||
| + | **During pregnancy the mucus is particularly thick (think lots of progesterone) and thus protective of the fetus. | ||
| + | |||
| + | *The ectocervix: | ||
| + | **The ectocervix is the juncture between the cervix and the vagina. | ||
| + | **The ectocervix is also called the '''portio vaginalis'''. | ||
| + | **At the ectocervix the '''epithelium changes from columnar (cervix) to stratified squamous (vagina)''' abruptly. | ||
| + | **The ectocervix is a common site for cell growth abnormalities like '''dysplasias, neoplasias, and invasive carcinomas'''. | ||
| + | **Normal ecotcervix: | ||
| + | ***http://pathweb.uchc.edu/eAtlas/Images/GYN/5764b.gif http://pathweb.uchc.edu/eAtlas/Images/GYN/5766b.gif | ||
| + | **http://www.nature.com/nri/journal/v8/n6/images/nri2302-f1.jpg | ||
| + | **http://www.arabicobgyn.net/doc/CERVIX_files/image010.gif | ||
| + | **http://www.path.cam.ac.uk/Abnormal/NP_Neoplasia/ME_Metaplasia/CX_Cervix/A_NP_ME_CX_01small.jpg | ||
| + | |||
| + | |||
| + | http://www.siumed.edu/~dking2/erg/images/RE052b.jpg | ||
| + | |||
| + | http://www.netterimages.com/images/vtn/000/000/007/7987-150x150.jpg | ||
| + | |||
| + | http://www.gfmer.ch/Books/Cervical_cancer_modules/Images/MI7.jpg | ||
| + | |||
| + | http://www.fpnotebook.com/_media/GynCervicalColposcopyAcetowhite1.jpg | ||
| + | |||
| + | http://missinglink.ucsf.edu/lm/IDS_106_LowerGI/IDS_images_downsized/fig10.jpg | ||
| + | |||
| + | ===Vagina=== | ||
| + | *The vagina has the standard four layers for an epithelial tract: mucosa, lamina propria, muscularis, and serosa (adventitia). | ||
| + | *The mucosa is characterized by stratified, squamous, non-keratinized epithelium. | ||
| + | **The epithelial cells of the vagina--like those of the uterus--accumulate glycogen upon estrogen signaling. | ||
| + | *The vaginal lamina propria has '''no glands''', patches of '''lymphocytes''', and can have folds. | ||
| + | **Recall, however, that the uterus does have glands in the lamina propria. | ||
| + | *The vaginal muscularis has '''interlacing bundles of smooth muscle'''. | ||
| + | |||
| + | http://www.lab.anhb.uwa.edu.au/mb140/CorePages/FemaleRepro/Images/vag02he.jpg | ||
| + | |||
| + | http://www.ansci.wisc.edu/jjp1/ansci_repro/lec/lec1/female_images/images_label/vagina(l).jpg | ||
| + | |||
| + | http://www.ouhsc.edu/histology/Glass%20slides/22_05.jpg | ||
| + | |||
| + | http://www.ouhsc.edu/histology/Glass%20slides/23_04.jpg | ||
| + | |||
| + | ===Mammary glands=== | ||
| + | *The mammary glands are made of a compound tubuloalveolar system; that is, there are alveoli that take part in the secretory component and there are ducts that take part in the transport component. | ||
| + | **A group of about 20 glands forms a '''mammary lobule'''. | ||
| + | *Secretory component: | ||
| + | **Milk is generated by '''cuboidal epithelial cells''' arranged in '''alveoli'''. | ||
| + | ***The alveoli develop as outgrowths of the ducts. | ||
| + | **Alveoli are surrounded by myoepithelial cells (that, upon oxytocin signaling, contract to move milk along the ducts). | ||
| + | ***The '''myoepithelial cells arise from the cuboidal epithelial cells'''. | ||
| + | **Plasma cells are found in and around the alveoli in order to '''generate IgA'''. | ||
| + | *Mammary ducts: | ||
| + | **The epithelium that lines the ductule system is '''stratified cuboidal'''. | ||
| + | **From the alveoli milk runs through '''lactiferous ducts''' to '''lactiferous sinuses''' and on to '''dilated reservoirs'''. | ||
| + | ***There is a significant amount of '''smooth muscle between the ducts and sinuses'''. | ||
| + | **Most breast cancers arise from lactiferous duct cells. | ||
| + | |||
| + | https://lh3.googleusercontent.com/_WdFQawAlzZM/TW_UdyeIT0I/AAAAAAAAAoA/pvQX_ngLS0M/s800/F22_27.jpg | ||
| + | |||
| + | http://www.nature.com/nrc/journal/v2/n2/images/nrc721-f1.jpg | ||
| + | |||
| + | http://www.genericlook.com/img/uploads/anatomy/mammary-glands.jpg | ||
| + | |||
| + | http://neuromedia.neurobio.ucla.edu/campbell/skin/wp_images/161_myoepithelial.gif | ||
| + | |||
| + | http://www.breast-cancer.ca/images/breast-myoepithelial-cells.jpg | ||
| + | |||
| + | http://neuromedia.neurobio.ucla.edu/campbell/glands/wp_images/myoepithelial%20cells.jpg | ||
| + | |||
| + | http://img.medscape.com/pi/emed/ckb/pediatrics_cardiac/1331339-1331345-1835675-1835738.jpg | ||
| + | |||
| + | ====Mammary glands at puberty==== | ||
| + | *Before puberty, the lactiferous ducts have formed but no alveoli exist. | ||
| + | *When '''estrogen''' increases at puberty ('''and prolactin is present'''), '''alveolar buds develop and regress''' with each ovarian cycle. | ||
| + | *Note that these alveolar buds are not full alveoli. | ||
| + | |||
| + | ====Mammary glands in pregnancy==== | ||
| + | *Upon pregnancy, estrogen is found at high levels '''along with prolactin, placental lactogen, and progesterone''' and therefore the alveolar ducts and alveoli fully develop. | ||
| + | *There are then two stages of milk production; lactogenesis is the initial production of milk while galactopoiesis is the continued production of milk. | ||
| + | *'''Lactogenesis is regulated by estrogen, progesterone, and prolactin'''. | ||
| + | **This makes sense because estrogen and progesterone increase throughout pregnancy and once progesterone and estrogen drop (at parturition), prolactin has its most potent effect. | ||
| + | *'''Galactogenesis is maintained by prolactin and oxytocin'''. | ||
| + | |||
| + | http://www.as.miami.edu/chemistry/2086/chap28/NewChap28-Female_files/image010.jpg | ||
| + | |||
| + | https://lh4.googleusercontent.com/_WdFQawAlzZM/TaOd4WAHBbI/AAAAAAAAAuc/9Hh5a4tSLKE/s800/mammary_gland_comparison.jpg | ||
| + | |||
| + | ====Breast milk==== | ||
| + | *The first milk generated is called colostrum; colostrum is '''lactoprotein- and immunoglobulin- rich''' and '''lipid-deficient'''. | ||
| + | *Lactation can generate 1100 to 2100 ml every day. | ||
| + | **Note that physio said 800-1200 ml / day. | ||
| + | *Recall that the cuboidal epithelial cells of the alveoli generate milk. | ||
| + | *These cuboidal epithelial cells use several secretion mechanisms to release their products. | ||
| + | **'''Merocrine secretion''' is used to secrete casein, alpha-lactalbumin, and PTH-RP. | ||
| + | **'''Apocrine secretion''' is used to secret TAGs and cholesterol. | ||
| + | **'''Exocytosis''' is used to secrete lactose. | ||
| + | **'''Transcytosis''' (from adjacent plasma cells) is used to secrete dimeric IgA. | ||
| + | |||
| + | ====Regulation of milk let-down==== | ||
| + | *Milk "let-down" is the release of milk from the alveoli to the ductule system. | ||
| + | *Let down is stimulated by suckling at the nipple which stimulates an afferent neuronal signal to the posterior pituitary (neurohypophysis) where neurons release an efferent hormonal signal (oxytocin) that stimulates the myoepithelial cells to contract and force milk distally through the tract. | ||
| + | **Note that '''afferent CNS signals also stimulate dopamine inhibition''' such that '''prolactin is increased''' which stimulates the cuboidal epithelial cells of the alveoli to increase milk production. | ||
| + | *Note that '''multiple neuroendocrine factors''' have been found besides oxytocin to '''relax the smooth muscle sphincter''' between the lactiferous ducts and the lactiferous sinuses. | ||
| + | |||
| + | ===Summary=== | ||
| + | *FSH stimulates follicle development in the ovary. | ||
| + | *Estrogens increase as the follicle develops and: | ||
| + | **inhibit FSH at the pituitary | ||
| + | **stimulate LH at the pituitary | ||
| + | *LH surge stimulates ovulation | ||
| + | *LH promotes corpus luteum formation | ||
| + | *Corpus luteum produces progesterone and estrogen | ||
| + | **Estrogen causes uterine proliferation phase | ||
| + | **Progesterone causes uterine secretory phase | ||
| + | *Progesterone inhibits LH | ||
| + | |||
| + | |||
| + | *Without implantation: | ||
| + | **Corpus luteum degenerates for lack of LH | ||
| + | **Progesterone and estrogen levels decrease | ||
| + | **Menstruation | ||
| + | |||
| + | |||
| + | *With implantation: | ||
| + | **Chorionic gonadotropin maintains corpus luteum (maintains estrogen and progesterone) | ||
| + | **Uterus remains in secretory phase for pregnancy. | ||
Revision as of 00:42, 12 April 2011
- started here on 03/28/11.
Contents |
Female reproductive histology
Ovarian cycle
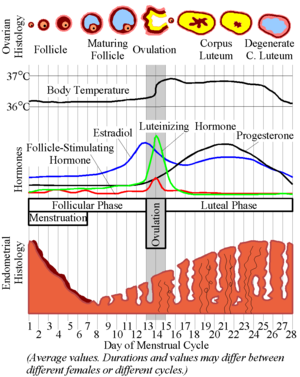
- The ovarian cycle describes the hormonal, anatomical, and reproductive changes that occur on a regular basis as the ovary generates a mature gamete for potential fertilization.
- The ovarian cycle coincides with the uterine cycle (which describes the hormonal and anatomical changes that conditions the reproductive tract for hosting an embryo).
- The ovarian cycle is primarily focused on the anatomical changes of the ovary (which contains the germ cells) and the changes in LH, FSH, estrogen, and progesterone.
Origin and fate of ovarian follicles
- Female gametes are generated from primordial germ cells in the ovaries, using a structure called the follicle.
- Ovarian follicles are composed of a germ cell (oocyte) surrounded by supporting cells (follicular epithelial cells).
- Ovarian follicle follicular epithelial cells include granulosa and theca cells.
- Primordial germ cells migrate originate from the yolk-sac (endoderm) and migrate to the genital ridge where the ovaries are developing.
- Note that this it makes sense that the germ cells have to migrate to the site of ovary development because they are of two different origisn: germ cells from yolk-sac endoderm and epithelium.
- Follicles undergo proliferation and reach their maximum number Follicles first develop at the genital ridges.
- There are approximately 3.5 million oocytes, 1 million oocytes, and 0.5 million oocytes at the fetal, neonatal, and puberty stages of development.
Ovarian anatomy
- The ovaries have cortex (outer) and medulla (inner) compartments.
- The cortex epithelium of the ovary is simple cuboidal epithelium.
- The cortex is the location of follicles surrounded by connective tissue and fibroblasts that make up the stroma.
- The medulla is the vascular core.


Ovarian follicle
- The follicle is a structure of follicular epithelia that surrounds the oocyte.
- Epithelial follicular cells proliferate throughout the follicular phase of the ovarian cycle.
- During the ovarian follicular phase mesenchymal cells will differentiate into theca cells to surround the follicle with an extra two layers.
- Theca cells of mesenchymal origin provide an inner endocrine layer of cells and outer vascular layer of cells.
- The endocrine layer of theca cells is called the theca interna; the vascular layer of theca cells is called the theca externa.
- The ovarian follicle has a specific anatomy of layers:
- The oocyte is at the center with a dense nucleolus, condensed chromosomes, many perinuclear mitochondria, and a fair amount of cytoplasm.
- The oocyte is surrounded by a dense layer called the zona pellucida (which will play an important role in fertilization)
- The zona pellucida is surrounded by follicular cells called granulosa cells which will be mitotic in the follicular phase
- Within the follicular cell population one may find a Call-Exner body which are collections of granulosa cell membrane with granulosa secretions within.
- The follicular cells are surrounded by a basement membrane (basal lamina).
- The basal lamina is surrounded by theca cells (from mesenchyme) which form two layers: theca interna and theca externa.
- Finally, the entire follicle with theca cell layers is surrounded by connective tissue of the ovary.




Stages of the ovarian follicle
- Recall that the ovarian follicle includes the oocyte and surrounding supporting follicular epithelial cells.
- The follicle begins as a primordial follicle, undergoes changes that facilitate maturation of the oocyte.
- Changes to the follicle include proliferation of the epithelial cells (granulosa cells), formation of a basement membrane, formation of the zona pellucida, and formation of the thecal layers.
- There are 4 stages (for our purposes) of follicular development: primordial follicle, developing follicle, secondary follicle, mature follicle.
- Eventually the follicle ejects the oocyte in a process called ovulation.
- After ovulation the follicle has several potential fates: atresia and differentiation into a corpus luteum.
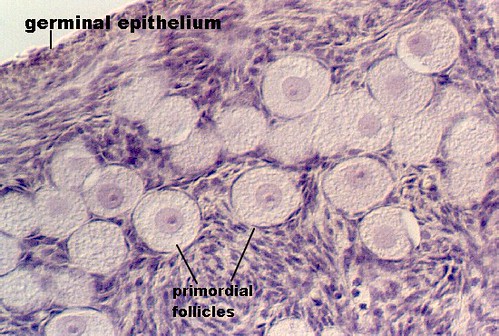
- Primordial follicle:
- The primordial follicle' contains a primordial germ cell and is surrounded by a single layer of follicular epithelial cells.
- Note that the follicular cells are squamous but are not yet considered granulosa cells.
- The primordial follicle is uniquely defined by having only a single layer of follicular epithelial cells.
- The germ cell of the primordial follicle is arrested in prophase of meiosis 1 and is therefore 4N with condensed, crossed-over chromosomes.
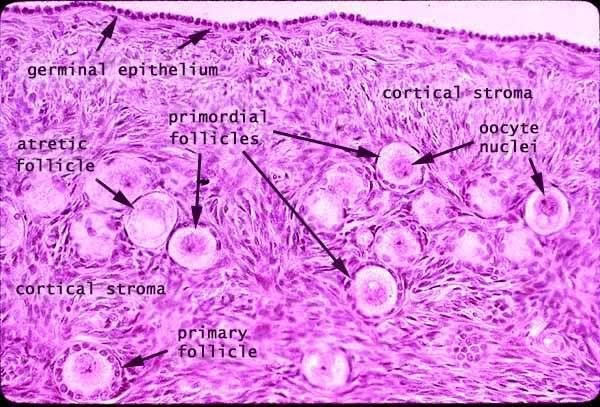
- Developing follicle:
- The developing follicle is uniquely defined by a basal lamina, a forming zona pellucida, multiple layers of granulosa cells and a theca interna.
- In the developing follicle, the follicular cells are cuboidal and have proliferated and differentiated into granulosa cells.
- Recall that theca cells arise from the stroma of the ovary--a source of mesenchymal cells.
- The zona pellucida is composed of glycoproteins and polysacchardies from both the granulosa cells and the oocyte.
- Note that communication to the oocyte can occur through cytoplasmic processes that extend form the zona pellucida into the oocyte.
- Secondary follicle:
- Secondary follicles are also called atral and vesicular follicles.
- The secondary (vesicular, antral) follicle is uniquely defined by a developing antrum and a theca externa.
- Clearly this makes sense with names like antral follicle or vesicular follicle.
- Granulosa cells reach their mature state in the secondary follicle and serve several purposes:
- Granulosa cells communicate with the oocyte via gap junctions.
- Granulosa cells contribute to the zona pellucida (think glycoproteins and polysaccharides).
- Granulosa cells produce the follicular fluid that fills the antrum.
- Follicular fluid is filled with hormone binding proteins (like SHBG) and will thus become an important source of hormones for oocyte development and then pregnancy maintenance.
- Granulosa cells converte androstendione to estradiol (via aromatase).
- Granulosa cells secrete stroma-weakening factors to allow expansion of the follicle.
- A primary stroma-weakening factor is plasminogen-activator which converts plasminogen to plasmin (fibrinolysin, a trypsin-like enzyme) which cuts up fibrin.
- Granulosa cells secrete a meiosis-regulationg factors.
- Granulosa cells secrete both a pro-meiosis factor and an anti-meiosis factor to promote movement from prophase 1 to metaphase 2 in the oocyte--no more and no less.
- Recall that the theca interna is considered the endocrine layer of thecal cells.
- Theca cells of the theca interna produce androstendione.
- Androstenedione from the theca interna cells is converted to estradiol by the granulosa cells.
- It is in the secondary follicle stage (antral stage, vesicular stage) that the oocyte reaches its mature size.

- Mature follicle:
- Mature follicles are also called Graafian follicles.
- The mature follicle is uniquely defined by the corona radiata and the cumulus oophorus.
- The corona radiata is a layer of granulosa cells that surrounds the zona pellucida of the oocyte along the antral aspect. The corona radiata is sometimes called the rim.
- The cumulus oophorus is a layer of granulosa cells that attaches the zona pellucida (and therefore the oocyte) to the membrana granulosa--the antral-surrounding layer of granulosa cells. The cumulus oophorus is sometimes called the stalk.
- Mature follicles are very large: can be over 1 cm!
- As a mature follicle, the oocyte progresses from prophase of meiosis 1 to metaphase of meiosis 2 and thus generates the first polar body.
- Note that having entered meiosis 2, the oocyte is called a secondary oocyte.
- Note that there are two physiological maturing processes occurring: the oocyte and the follicle but only the follicle maturity can be seen histologically.

http://t0.gstatic.com/images?q=tbn:ANd9GcR_5ajvKIDofXIvPSq_8CEqUgDbjlsBRtYNqKEDaGYemdfQoqPAtQ

- Deciding on which type of follicle you're observing:
- flattened follicular cells: primordial
- cuboidal folliclar cells (with a layer on either side--zona pellucida or basal lamina): developing
- antrum / fluid: secondary follicle
- no way to distinguish secondary from mature.

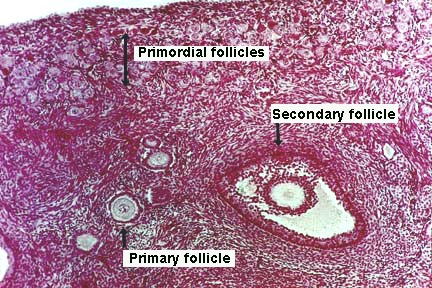
- Here is a good image (though it does not show a mature follicle):



Endocrine regulation of follicle maturation
- FSH from the anterior pituitary augments the maturation of follicles that are developing in the ovary.
- As one follicle becomes dominant, it produces follicular regulatory protein to inhibit growth of all other follicles.
Do the other follicles undergo atresia or just stop growing until the next round because of follicular regulatory protein.
- Recall that granulosa cells proliferate in the secondary stage of follicular development and that granulosa cells generate estrodiol from the androgens produced by interna theca cells.
- Increased estrogen inhibits FSH release at the pituitary thus stopping the growth of the follicle and allowing ovulation.
- Increased estrogen stimulates LH release at the pituitary thus commencing ovulation.
- Recall these classic images:

Ovulation
- Generally a single egg is released into from one of the two ovaries.
- As the granulosa cells of the secondary and mature follicle produce more and more estrogen, more and more LH is released from the anterior pituitary gland (adenohypophysis, pars distalis).
- Ovulation events include:
- Breakdown of the cumulus oophorus, thus the oocyte floats freely in the antrum and follicular fluid.
- Weakening of the ovarian stroma:
- Proteolytic enzymes like collagenase disrupt the stromal connective tissue.
- Granulosa cell connections weaken
- Local ischemia causes a pale spot on the surface of the ovary called a stigma.
- Follicular wall ruptures releaseing an oocyte with the corona radiata and zona pellucida surrounding.
The corpus luteum
- After the dominant ovarian follicle undergoes ovulation, the follicle may degenerate or become a temporary endocrine structure called the corpus luteum.
- The corpus luteum is a differentiation of the granulosa and theca cells in response to LH signaling.
What determines if the follicle becomes a corpus luteum? Something made by the placenta?
- LH causes granulosa cells to become granulosa lutein cells.
- Granulosa lutein cells develop the morphology of a secretory cell and actively produce progesterone.
- Note that the production of progesterone by the granulosa lutein cells is necessary for implantation of the embryo.
- LH causes theca cells to become theca lutein cells.
- Theca lutein cells continue to produce androsteindione and other estrogen precursors.
- Note that a clot within the follicle vascularizes to perfuse the granulosa lutein cells that make up the center of the corpus luteum.
- If pregnancy does not occur, the corpus luteum is called the corpus luteum of menstruation.
- The corpus luteum of menstruation is maintained as long as LH is present.
- Recall, however, that the corpus luteum produces progesterone and that progesterone has an inhibitory effect on LH release by the pituitary.
- Therefore, progesterone from the corpus luteum is self limiting.
- That is, the corpus luteum will bring about self-demise via progesterioen inhibition of pituitary-LH unless chorionic gonadotropin is generated by the placenta.
- Without pregnancy, the corpus luteum lasts 10-14 days.
- If pregnancy occurs, the corpus luteum is called the corpus luteum of pregnancy.
- Recall that trophoblasts of the placenta produce chorionic gonadotropin.
- Granulosa cells of the corpus luteum of pregnancy produce relaxin which has a smooth-muscle relaxing effect (histo says "during parturition", wikipedia says "during gestation").
- Relaxin opposes the pro-parturition actions of oxytocin.
- Relaxin targets the fibrocartilage of the pubic symphysis to increase articulation.
- Note that physio notes say that the role of relaxin in pregnancy is unclear.

Follicular atresia
- Follicles can undergo atresia from any stage of follicular development (primordial, developing, secondary, or mature).
- Follicular atresia generates a long-lasting, scar-tissue structure called the corpus albicans.
- Note that the larges of the coprus albicans found in an ovary likely arose from a previous corpus luteum.

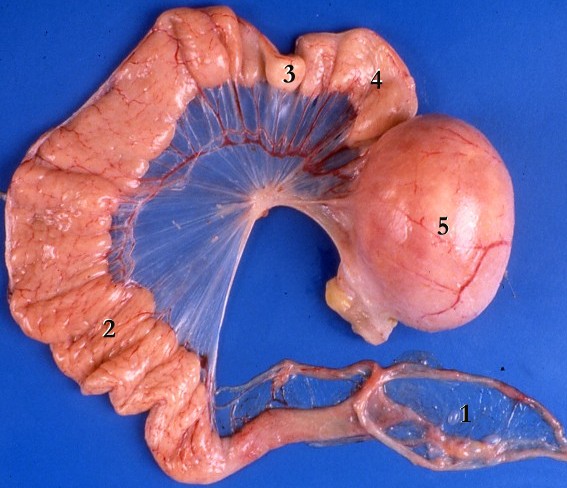
The uterine tubes
- The uterine tubes conduct the mature female gamete from the ovary to the uterus and are the site of fertilization.
- The uterine tubes can also be called oviducts or Fallopian tubes.
- The uterine tubes are muscular tubes that extend from the ovary on the posterolateral wall of the abdomen to the medioventral aspect of the abdomen and the lateral aspect of the uterus.
- The Fallopian tubes are approximately 12 cm long.
- There are four major sections to the oviducts from the ovary to the uterus: infundibulum, ampulla, isthmus, and interstitial segments.
- The infundibulum has fimbriae and "bears osteum.
What does "bears osteum mean"?
- The ampulsa is the dilated intermediate segment of the oviduct.
- The isthmus is the media 1/3 of the Fallopian tube.
- The interstitial segment pierces the uterine wall.
- As the oviducts progresses distally, there are fewer involdings.


http://www.jci.org/articles/view/29424/files/JCI0629424.f1/medium
Layers of the oviduct
- Like other epithelial tracts there are four major layers to the oviduct (from inner to outer): mucosa, lamina propria, muscularis, and serosa.
- Secretions from the oviduct promote sperm activation.
Does this refer to capacitation?
- Mucosa of the oviduct:
- The mucosa of the oviduct is comprised of columnar, ciliated epithelial cells.
- These columnar cells are secretory and are called Peg cells.
- Estrogen (from the corpus luteum) increases the height of the columnar cells.
- Progesterone (from the corpus luteum) increases the ciliary action of the columnar epithelial cells of the mucosa.




- Lamina propria:
- The lamina propria of the oviduct is highly vascularized.
- Fimbriae are especially concentrated with smooth muscle and become highly active around ovulation.

- Muscularis:
- As with so many muscularis layers, there is an inner circular and outer longitudinal layer.
- The two layers of the muscularis are interwoven.
- There is a peristaltic contraction movement toward the uterus.
- Note that one is unlikely to differentiate two layers in lab.

- Serosa:
- The serosa is a true serosa because it is lined with mesothelium.



The uterus
- The uterus is comprised of four parts (proximal to distal along the genital tract): the fundus, body, isthmus, and cervix.
- The fundus is the rounded superior end.
- The body is the main portion of the uterus.
- The isthmus is the constricted middle portion.
- The cervix is the cylindrical portion that projects into the vagina.
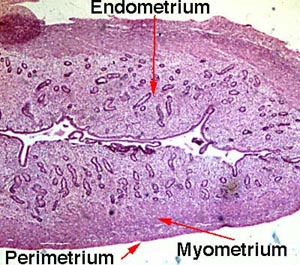
Layers of the uterine wall
- Like the oviducts and other epithelial tracts, there are four tissue-type layers to the uterus which make up three functional layers of the uterus.
- The tissue layers are (inner to outer): mucosa, smooth muscle, serosa, and adventitia.
- The functional layers are (inner to outer): endometrium (think implantation), myometrium (think contraction), and epimetrium.
- The endometrium is composed of mucosa.
- The myometrium is composed of smooth muscle.
- The epimetrium is composed of serosa and adventitia.
- Note that the cervix is histologically distinct from the rest of the uterus; we will revisit this.






- stopped here on 03/28/11.
- started here on 03/30/11.
The uterine cycle
- Recall that the ovarian cycle describes the hormonal, anatomical, and reproductive changes of the gonads while the uterine cycle describes the hormonal and anatomical changes to the genital tract (including the uterus).
- The uterine cycle is also called the endometrial cycle as it is the endometrial layer of the uterus that undergoes most of the changes during the uterine cycle.
- From physio notes:
- The phases of the menstrual cycle can also be described by the changes to the uterus (the reproductive tract).
- The uterine cycle of menstruation has four stages: the proliferative stage, secretory stage, ischemic stage, and menstrual stage.
- The proliferative stage is characterized by endometrium hypertrophy and formation of spiral arteries.
- Recall that the uterine proliferative stage occurs during the ovarian follicular phase.
- So as the ovary is maturing its follicle, the uterus is regenerating it's surface (where the egg will implant) and increasing vascular access to the surface.
- The secretory stage is characterized by coiling of glands, secretion of mucus, tortuous arteries, and peak thickness of the endometrium.
- Recall that the uterine secretory stage occurs during the ovarian luteal phase.
- So, as the ovary has shed an ovum and is now increasing hormone production via the corpus luteum, the uterus is using glands and arteries of the uterus to modify the uterine microenvironment to the optimal conditions for egg implantation.
- The ischemic stage is characterized by arterial constriction, decreased blood flow, and increased prostaglandins.
- Recall that the ischemic stage occurs during the ovarian menses phase.
- So as the ovary has reached its lowest levels of hormone production, the uterus is decreasing nutrition to the endometrium and allowing the mucosa to undergo necrosis by ischemia.
- The menstrual stage is characterized by desquamation of the endometrium.
- Recall that the menstrual stage occurs during the ovarian menses phase.
- So as the ovary has reached its lowest levels of hormone production, the uterus is shedding its endometrium.
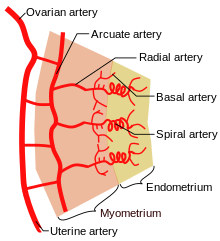
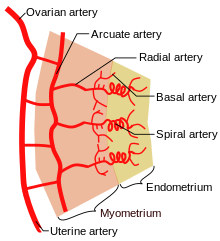
Uterine vasculature
- The primary changes of the uterine cycle are to the vasculature of the endometrium.
- Recall that the uterus is suspended from the lateral walls of the abdomen by the broad ligament which also serves to carry the vasculature of the uterus.
- The uterus is supplied by arcuate arteries that run along the myometrium layer and by radial arteries that cross into the endometrium.
- The radial arteries give off straight (basal) arteries that supply the endometrium basalis.
- Note that the endometrium is divided into two layers: the endometrium basalis is a constant, mostly unchanging layer while the endometrium functionalis cycles through generation (proliferation) and shedding.
- There is no structural marker to distinguish between the basalis and the functionalis of the endometrium.
- Spiral (coiled) arteries are heavily muscular, generated during the endometrial cycle, and bridge the radial arteries into the endometrial functionalis.
- Smaller arteries also exist off of the straight (basal) and spiral (coiled) arteries, including nutrient arterioles / capillaries, and venous sinusoids.
- Of special note are the vascular structures nearest the lumen of the uterus called lacunae.
Uterine endometrium
- Recall that the endometrium of the uterus contains the mucosa layer (of the four common epithelial layers: mucosa lamina propria, muscularis, and serosa).
- The endometrial mucosa contains uterine glands.
- Uterine glands are tubular with many branches.
- Uterine glands contain both ciliated and non-ciliated cells.

Histological changes in the uterine cycle
- Recall that there are four stages to the uterine cycle: menstruation, the proliferative stage, the secretory stage, and the ischemia stage.
- Note that we start with menstruation because in the ovary a new follicle is beginning to mature (follicular phase) so it seems like a good place to call the "start" in the gonads.
- The phases are divided over approximately 28 days: menstruation (days 1-5), proliferation (6-15), secretion (16-17), ischmia (18-28).
- Menstruation:
- Recall that during menstruation, the ovary is producing very little estrogen / progesterone and a follicle is in the beginning of its maturation.
- During menstruation, the endometrium functionalis is shed.
- Note that the base of the uterine glands remain visible in the endometrium basalis.
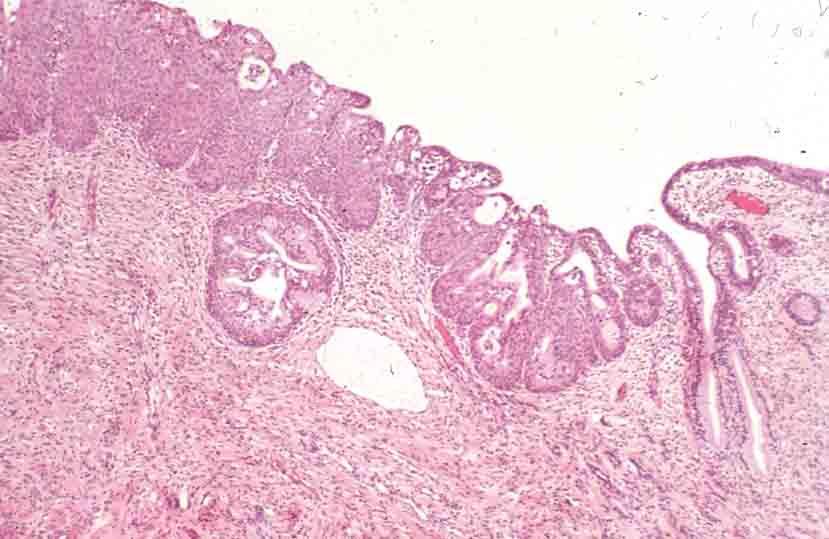
- Proliferative stage:
- Recall that during the proliferative stage, a follicle in the ovary is maturing to secondary and Graafian stage and producing more and more estrogen and progesterone.
- The proliferative stage is driven by estrogen produced by the developing follicle.
- The proliferative stage is characterized by resurfacing of the endometrium through epithelial and stromal proliferation.
- This resurfacing requires the lengthening of the uterine glands and is accompanied by coiling of the glands.
- In addition to gland coiling, spiral arteries develop in the thickening endometrium.
- Cells of the proliferative endometrium accumulate glycogen.
Why accumulate glycogen?
- Secretory stage:
- Recall that during the secretory stage the ovary has generated a corpus luteum and is producing estrogen and progesterone.
- Recall that the secretory stage takes place after ovulation and lasts until the corpus luteum degenerates or pregnancy is terminated.
- The secretory stage is driven by progesterone from the corpus luteum.
- The secretory stage is characterized by release of glycoprotein-rich products, swelling and torture of the glands and spiral arteries, and accumulation of fluid in the stroma of the endometrium.
- Ischemia:
- Recall that during the ischemic stage the ovary is seeing low hormone levels and the degeneration of the corpus luteum.
- Note that the ischemic stage does not occur when pregnancy is initiated by implantation and the placenta maintains estrogen and progesterone levels.
- The ischemic stage is characterized by constriction of the coiled arteries, stromal fluid loss, and lymphocyte / macrophage cell invasion.
- Recall that progesterone inhibits prostaglandins and that prostglandins are potent vasoconstrictors.
- When the corpus luteum degenerates and progesterone levels drop, local prostaglandins are released into the endometrium.
- The coiled arteries dilate and constrict intermittently which causes ischemia, cell lysis, a weakened stroma, bursting vessles, and debridement of the functionalis.
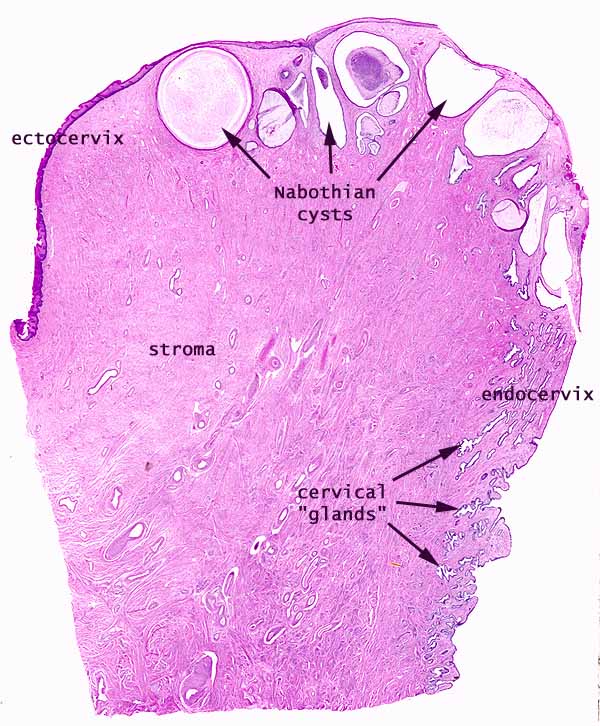
Uterine cervix
- As mentioned before, the cervix is histologically distinct from the rest of the uterus.
- The cervical mucosa:
- The cervical mucosa of the uterus is not shed at menstruation like it is along the rest of the uterus.
- The cervical myometrium:
- The cervical myometrium has less smooth muscle and abundant collagenous connective tissue with elastic fibers.
- The cervical endometrium:
- The cervical endometrium has denser stroma, simple columnar epithelium, branched, dilated, cyst-forming glands, and longitudinal mucosal folds called plicae (plicae palmatae).
- Cervical glands can form cysts called Nabothian cysts.
- The cervical endometrium has denser stroma, simple columnar epithelium, branched, dilated, cyst-forming glands, and longitudinal mucosal folds called plicae (plicae palmatae).
- The cervical mucus:
- The cervical mucus changes throughout the uterine cycle.
- Mid way through the cycle (think ovulation and sperm-friend environment) the mucus is watery, contain lysozyme (bacterioalcidal), and promotes sperm motility.
- This sperm-friendly mucus is estrogen-stimulated.
- Late in the uterine cycle (think corpus luteum and potential implantation) the mucus is viscous and progesterone-stimulated.
- During pregnancy the mucus is particularly thick (think lots of progesterone) and thus protective of the fetus.
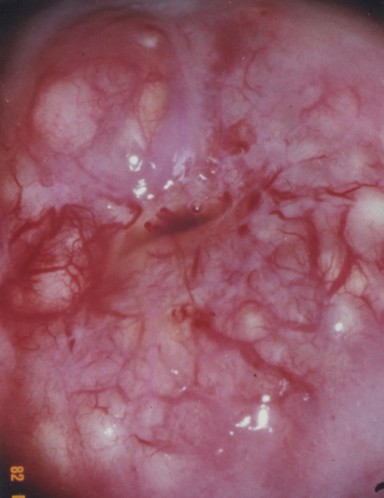
- The ectocervix:
- The ectocervix is the juncture between the cervix and the vagina.
- The ectocervix is also called the portio vaginalis.
- At the ectocervix the epithelium changes from columnar (cervix) to stratified squamous (vagina) abruptly.
- The ectocervix is a common site for cell growth abnormalities like dysplasias, neoplasias, and invasive carcinomas.
- Normal ecotcervix:





Vagina
- The vagina has the standard four layers for an epithelial tract: mucosa, lamina propria, muscularis, and serosa (adventitia).
- The mucosa is characterized by stratified, squamous, non-keratinized epithelium.
- The epithelial cells of the vagina--like those of the uterus--accumulate glycogen upon estrogen signaling.
- The vaginal lamina propria has no glands, patches of lymphocytes, and can have folds.
- Recall, however, that the uterus does have glands in the lamina propria.
- The vaginal muscularis has interlacing bundles of smooth muscle.

.jpg)


Mammary glands
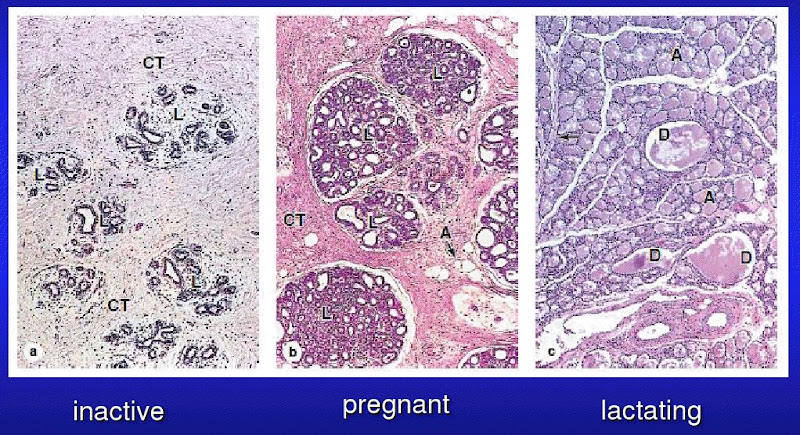
- The mammary glands are made of a compound tubuloalveolar system; that is, there are alveoli that take part in the secretory component and there are ducts that take part in the transport component.
- A group of about 20 glands forms a mammary lobule.
- Secretory component:
- Milk is generated by cuboidal epithelial cells arranged in alveoli.
- The alveoli develop as outgrowths of the ducts.
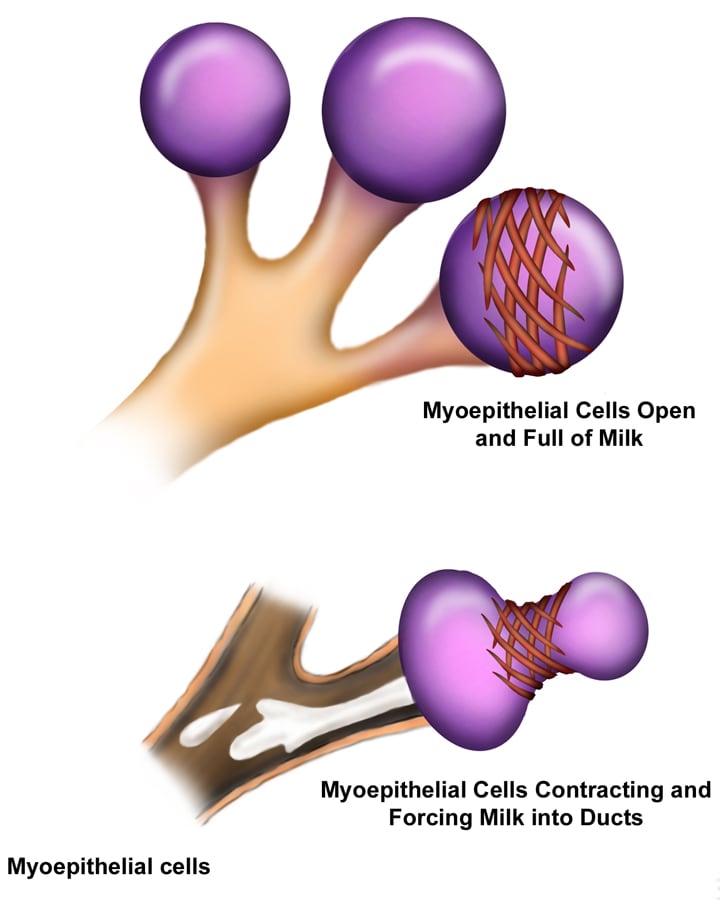
- Alveoli are surrounded by myoepithelial cells (that, upon oxytocin signaling, contract to move milk along the ducts).
- The myoepithelial cells arise from the cuboidal epithelial cells.
- Plasma cells are found in and around the alveoli in order to generate IgA.
- Milk is generated by cuboidal epithelial cells arranged in alveoli.
- Mammary ducts:
- The epithelium that lines the ductule system is stratified cuboidal.
- From the alveoli milk runs through lactiferous ducts to lactiferous sinuses and on to dilated reservoirs.
- There is a significant amount of smooth muscle between the ducts and sinuses.
- Most breast cancers arise from lactiferous duct cells.






Mammary glands at puberty
- Before puberty, the lactiferous ducts have formed but no alveoli exist.
- When estrogen increases at puberty (and prolactin is present), alveolar buds develop and regress with each ovarian cycle.
- Note that these alveolar buds are not full alveoli.
Mammary glands in pregnancy
- Upon pregnancy, estrogen is found at high levels along with prolactin, placental lactogen, and progesterone and therefore the alveolar ducts and alveoli fully develop.
- There are then two stages of milk production; lactogenesis is the initial production of milk while galactopoiesis is the continued production of milk.
- Lactogenesis is regulated by estrogen, progesterone, and prolactin.
- This makes sense because estrogen and progesterone increase throughout pregnancy and once progesterone and estrogen drop (at parturition), prolactin has its most potent effect.
- Galactogenesis is maintained by prolactin and oxytocin.

Breast milk
- The first milk generated is called colostrum; colostrum is lactoprotein- and immunoglobulin- rich and lipid-deficient.
- Lactation can generate 1100 to 2100 ml every day.
- Note that physio said 800-1200 ml / day.
- Recall that the cuboidal epithelial cells of the alveoli generate milk.
- These cuboidal epithelial cells use several secretion mechanisms to release their products.
- Merocrine secretion is used to secrete casein, alpha-lactalbumin, and PTH-RP.
- Apocrine secretion is used to secret TAGs and cholesterol.
- Exocytosis is used to secrete lactose.
- Transcytosis (from adjacent plasma cells) is used to secrete dimeric IgA.
Regulation of milk let-down
- Milk "let-down" is the release of milk from the alveoli to the ductule system.
- Let down is stimulated by suckling at the nipple which stimulates an afferent neuronal signal to the posterior pituitary (neurohypophysis) where neurons release an efferent hormonal signal (oxytocin) that stimulates the myoepithelial cells to contract and force milk distally through the tract.
- Note that afferent CNS signals also stimulate dopamine inhibition such that prolactin is increased which stimulates the cuboidal epithelial cells of the alveoli to increase milk production.
- Note that multiple neuroendocrine factors have been found besides oxytocin to relax the smooth muscle sphincter between the lactiferous ducts and the lactiferous sinuses.
Summary
- FSH stimulates follicle development in the ovary.
- Estrogens increase as the follicle develops and:
- inhibit FSH at the pituitary
- stimulate LH at the pituitary
- LH surge stimulates ovulation
- LH promotes corpus luteum formation
- Corpus luteum produces progesterone and estrogen
- Estrogen causes uterine proliferation phase
- Progesterone causes uterine secretory phase
- Progesterone inhibits LH
- Without implantation:
- Corpus luteum degenerates for lack of LH
- Progesterone and estrogen levels decrease
- Menstruation
- With implantation:
- Chorionic gonadotropin maintains corpus luteum (maintains estrogen and progesterone)
- Uterus remains in secretory phase for pregnancy.


