Chapter 26 notes (Renal)
From Biol557
(Difference between revisions)
149.166.133.197 (Talk)
(Created page with '==The urinary system== ===An introduction to the urinary system=== *The urinary system removes most of the physiological waste from the body. *We'll talk about the organization o…')
Newer edit →
(Created page with '==The urinary system== ===An introduction to the urinary system=== *The urinary system removes most of the physiological waste from the body. *We'll talk about the organization o…')
Newer edit →
Revision as of 16:19, 17 March 2010
The urinary system
An introduction to the urinary system
- The urinary system removes most of the physiological waste from the body.
- We'll talk about the organization of the kidney and how it removes waste.
- We'll talk about how urine concentration and volume is controlled.
Consisting of the kidneys, ureters, urinary bladder, and urethra, the urinary system has three primary functions
- There are three major functions of the urinary system:
- Excretion: the removal of organic waste products from the body fluids; performed by the kidneys.
- Elimination: the discharge (urination, micturition) of wastes from the body; performed by the ureters, bladder, and urethra.
- Homeostatic regulation of the volume and solute concentration of the blood plasma: performed by the kidneys in conjunction with endocrine (and nervous system?) control.
- The urinary system has several other functions:
- Regulating blood volume and blood pressure.
- Regulating plasma concentrations of sodium, potassium, chloride, calcium, and other ions.
- Helping to stabilize blood pH by controlling the loss of hydrogen ions and bicarbonate ions in urine.
- Conserving valuable nutrients, by preventing their excretion in urine.
- Assisting the liver in detoxifying poisons and deaminating amino acids for metabolism by other tissues.
- All of these processes are tightly regulated and if neglected can be deadly.
Kidneys are highly vascular structures containing functional units called nephrons, which perform filtration, reabsorption, and secretion
- The kidneys lie on either side of the vertebral column.
- There are three mechanisms that stabilize the kidneys in their location:
- the overlying peritoneum,
- contact with neighboring visceral organs, and
- supporting connective tissues.
- The connective tissues that support and protect the kidneys can be broken down into three layers:
- The fibrous capsule lies closest to the kidney and covers the whole organ.
- The perinephric fat capsule is a thick layer of adipose tissue that surrounds the fibrous capsule.
- The renal fascia is a layer of connective tissue that connects to the fibrous capsule of the kidney, to the muscular wall of the thoracic cavity to the posterior, and to the peritoneum to the anterior, thus anchoring the kidney in position.
- Detachment of the kidney from its anchored position can place the kidney at risk for easy injury upon bumping or jarring.
- Adult kidneys are about 10cm by 5.5cm.
- The hillum is the indentation where the renal artery and renal nerves enter the kidney and where the portal vein and ureter exit the kidney.
Sectional anatomy of the kidney
- The fibrous capsule that covers the outside of the kidney also attaches to the outer-most structures just inside the kidney.

- Urine drains from the papilla into minor calyces which make up major calyces which make up the renal pelvis which drains into the ureter.
- Urine production begins at the nephrons which are located in the cortex of each renal lobe and number about 1.25 million.
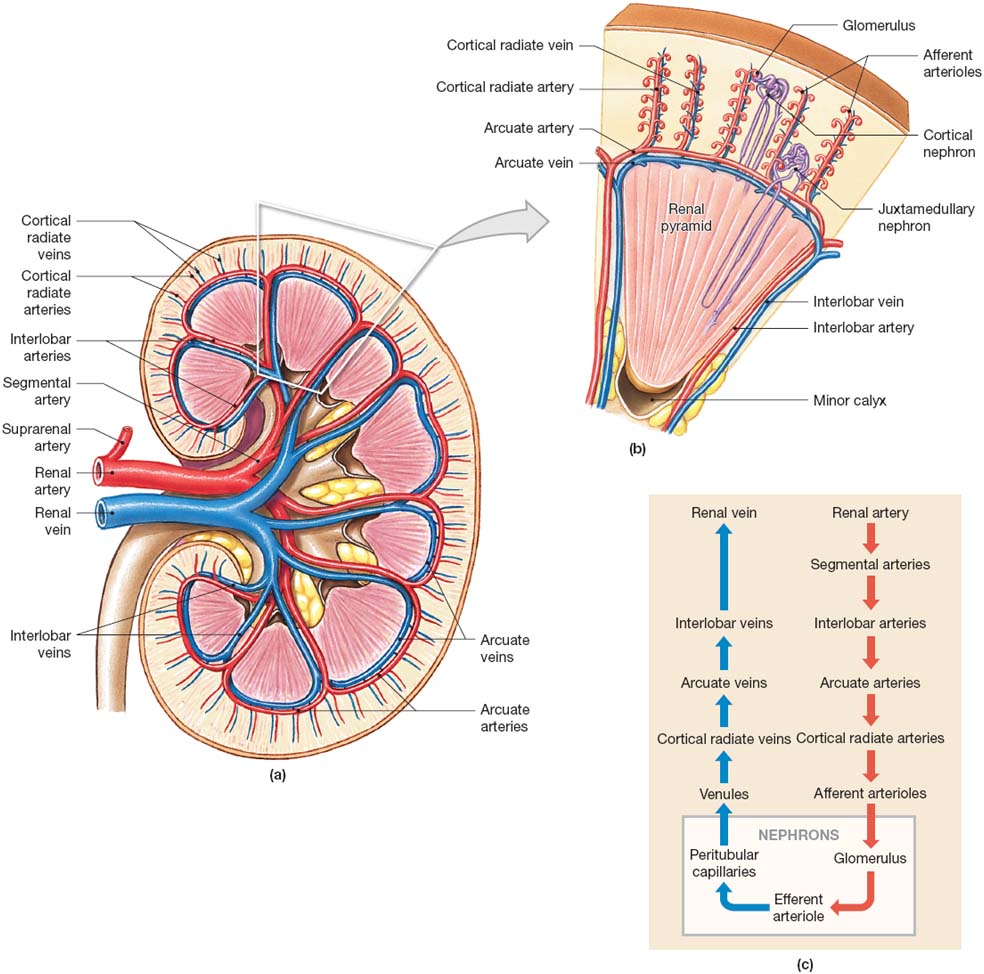
Blood Supply and Innervation of the Kidneys
- Tons of blood flows through the kidneys: 20-25% of one's cardiac output, about 1.2 liters per minute!
- The renal artery enters the kidney and the divides into smaller and smaller segments which ultimately provide nutrients to the individual nephrons before they join back together to form the renal vein.
- Renal invervation consists of a nerve that enters at the hillum and follows the pathways of the renal artery.
- The nerves of the kidney are primarily sympathetic.
- The nerves of the kidney:
- Adjusts rates of urine production by changing the blood pressure at the kidney and the amount of blood flow.
- Stimulates the release of renin which ultimately retains water and salt from the urine by stimulating enhanced reabsorption.
Clinical note: Analysis of renal blood flow
- Because PAH (para-aminohippuretic acid) is nearly completely removed from the blood at the kidney, one can measure the renal blood flow by administering it into the blood and comparing concentrations of PAH in the blood plasma and the urine.
- However, it is usually easier to just measure the glomerular filtration rate.
The Nephron
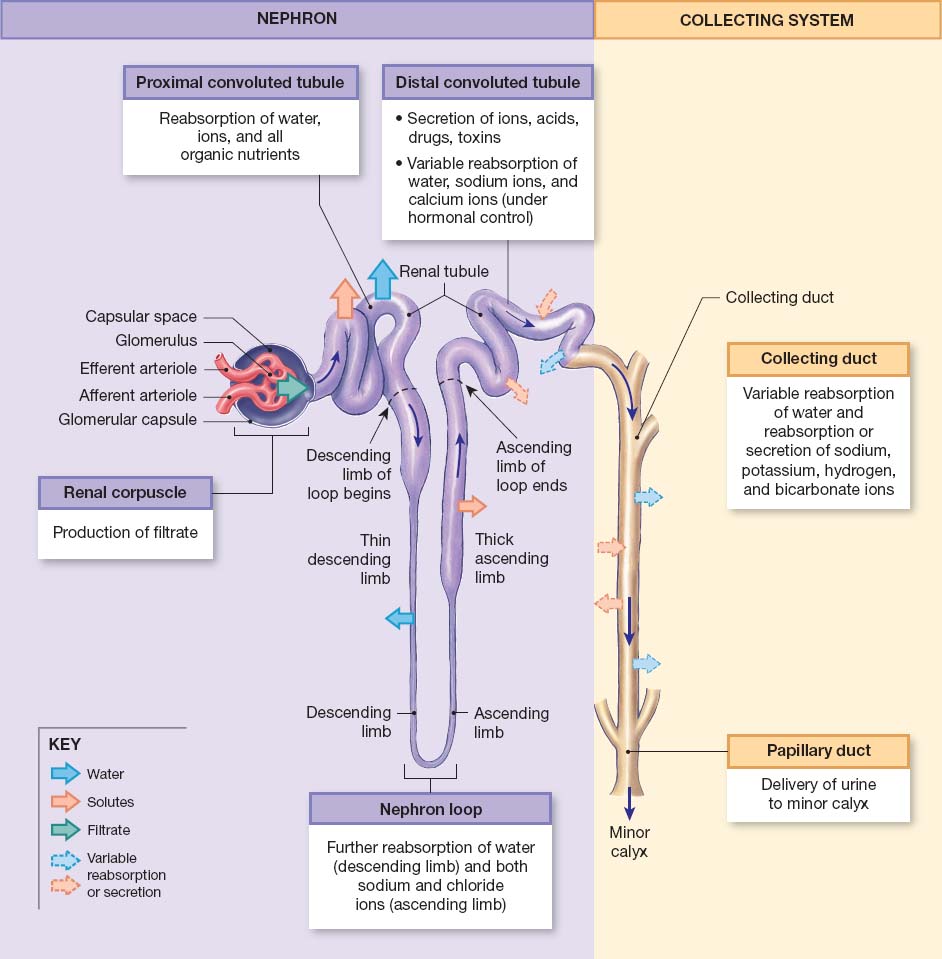
- Blood comes through the afferent arteriole to the renal corpuscle, then continues through the glomerulus and the capillaries there. Blood then leaves the glomerulus through the efferent arteriole, to the peritubular capillaries, and on to the venous system.
- The filtrate that leaves the blood into the nephron at the renal corpuscle is essentially protein-free.
- Filtrate enters the renal tubules where three things occur:
- Reabsorption of 90% of the water in the filtrate,
- Reabsorption of all the useful organic nutrients,
- Secretion of any remaining waste products that weren't filtered at the glomerulus.
- Once filtrate has entered the renal tubules it is also called tubular fluid.
- Remember that the tubular fluid is going to become urine, so when we say that some part of the nephron reabsorbs something we mean that the entity comes out of the tubular fluid (that is, urine) back into the body. Therefore, reabsorbed stuff will not be excreted.
- There are subregions to the renal tubules, each with a particular function:
- The proximal convoluted tubules: serve to reabsorb ions, organic molecules, vitamins and water while secreting drugs, toxins, and acids.
- The loop of Henle (nephron loop):
- The descending loop reabsorbs water.
- The ascending loop reabsorbs ions and helps form a concentration gradient in the medulla.
- The distal convoluted tubules: reabsorb sodium and calcium and secrete drugs, ammonia, toxins, and acids.
- Nephrons empty their tubular fluid into collecting ducts, which begin in the cortex, travel to the medulla, and empty into papillary ducts which drain into the minor calyx (which form major calyces, etc.).
- There are two types of nephrons: cortical nephrons and juxtamedullary nephrons.
- Though the cortical nephrons outnumber the juxtamedullary nephrons and therefore are responsible for most the fitration of the blood, it is the juxtamedullary nephrons that are responsible for generating concentrated urine.
- These two types of nephrons differ in the length of the nephron loop (juxtamedullary nephrons have much longer loops that extend into the medulla) and in the vasculature that follow the renal tubules.

The renal corpuscle
- The glomerular capsule surrounds the capillaries of the corpuscle and connects the fluid to the opening of the renal tubules.
- The outerwall of the corpuscle is made of a simple squamous cell wall.
- Podocytes are specialized cells of the visceral wall of the corpuscle that extend their foot-like processes onto the areas of the capillaries where filtrate passes through. Podocytes serve as a mesh through which filtrate must be small enough to pass.
- Mesangial cells sit between the capillaries and can respond to angiotensin II, vasopressin, and histamine in order to change the diameter of the capillaries, thus changing the rate of capillary blood flow.
- Fenestrated: "Having windows" per wiktionary.
- The capillaries at the glomerulus are fenestrated to allow lots of stuff to flow out.
- The filtration membrane is made up of the podocyte processes, the fenestrated endothelium of the capillaries, and the dense layer of the capillaries.
- While filtration is passive and effective, many useful molecules that we'd like to keep pass into the tubular fluid along with the many waste molecules that we don't want to keep.
Clinical note: Glomerulonephritis
- Glomerulonephritis is an inflammation of the glomerulus.
- Any condition that causes a massive immune response can cause this condition which leads to decreased filtration at the glomerulus.
- This disorder is caused by the clogging of the glomerulus by antibodies, which are small enough to get through the dense layer but too large to get through the podocyte processes.
The proximal convoluted tubule
- The peritubular fluid surrounds the proximal convoluted tubule.
- The cells of the proximal convoluted tubule (PCT) have microvilli on their apical surface.
- The function of the PCT is primarily absorption but can do some secretion.
- The PCT absorbs organic nutrients, ions, water, and plasma proteins (if present).
- The PCT deposits its absorbants into the peritubular fluid.
The nephron loop
- Each limb (think "ascending" and "descending") contains a thick and thin segment; this refers to the thickness of the cells making up the wall, not to the diameter of the lumen.
- The wall of the thick segment is made up of cuboidal epithelial cells while the thin walls are made of squamous epithelial cells.
- The thick, descending loop pumps sodium and chloride ions out of the tubular fluid (which is especially noticeable in the juxtamedullar nephrons where extraordinarily high concentrations of ions are found in the peritubular fluid).
- The thin descending loop is permeable to water but not to solutes and therefore water moves from the tubular fluid to the peritubular fluid which serves to concentrate the tubular fluid (urine).
The distal convoluted tubule
- The distal convoluted tubule (DCT) has smaller a smaller diameter than the PCT and does not have microvilli on the apical surface.
- There are three important functions that occur at the DCT:
- the active secretion of ions, drugs, toxins, and acids,
- the selective reabsorption of sodium and calcium (helpful in regulating concentrations of these two ions in the blood plasma),
- the selective reabsorption of water (helpful in regulating concentration of urine).
Is it really the concentration of urine we care about or the regulation of blood volume and ion concentration?
- The juxtaglomerular complex:
- This complex is made up of the macular densa and the juxtaglomerular cells.
- The juxtaglomerular complex is responsible for secreting erythropoietin and renin.